Florida Medicaid’s Managed Medical Assistance Program
Contents
- What is the Managed Medical Assistance Program?
- How does the program work?
- What are the benefits of the program?
- How can I enroll in the program?
- What is the coverage under the program?
- What are the eligibility requirements for the program?
- What are the managed care plans offered under the program?
- How do I choose a managed care plan?
- How do I change my managed care plan?
- What are the rights and responsibilities of enrollees?
Florida Medicaid’s Managed medical assistance Program (MMAP) is a managed care program that provides health care coverage for eligible low-income adults and children. MMAP members receive benefits and services through a Medicaid health plan.
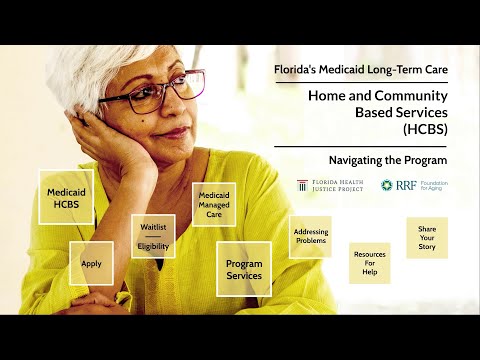
Checkout this video:
What is the Managed Medical Assistance Program?
The Managed Medical Assistance Program (MMAP) is a program within Florida Medicaid that provides health care coverage to eligible low-income adults, children, pregnant women, and people with disabilities. The program is managed by the Florida Department of Health and Human Services.
MMAP provides comprehensive health care benefits, including primary and preventive care, hospitalization, prescription drugs, and mental health services. beneficiaries also have access to community-based services, such as case management, transportation assistance, and home health services.
Enrollment in MMAP is voluntary for most people; however, some groups of beneficiaries are required to enroll in the program. These include people who are enrolled in the Temporary Assistance for Needy Families (TANF) program and people who are involuntarily committed to a state mental hospital.
If you are eligible for MMAP, you can choose to enroll in any one of the participating health plans. To find a list of participating health plans in your area, please visit the Florida Medicaid website or contact your local Medicaid office.
How does the program work?
Florida Medicaid’s Managed Medical Assistance (MMA) program is a health care delivery system that contracts with managed care organizations (MCOs) to provide comprehensive, cost-effective health care services to eligible Medicaid recipients.
MMA eligibility is determined by the Florida Department of Children and Families (DCF). To be eligible for MMA, an individual must be:
-A resident of the state of Florida
-A U.S. citizen or legal alien
-In need of medical assistance
-Between the ages of 0 and 65
-Have an annual income at or below 133% of the federal poverty level (FPL)
Individuals who are not eligible for Medicaid but who meet certain other criteria may be eligible for MMA through the Low Income Pool (LIP) program. To be eligible for LIP, an individual must be:
-A resident of the state of Florida -A U.S. citizen or legal alien -In need of medical assistance -Between the ages ghbv 0 and 65 -Have an annual income at or below 200% of the FPL
What are the benefits of the program?
The Florida Medicaid’s Managed Medical Assistance Program (MMAP) is a state-wide program that provides health care coverage for low-income adults, children, pregnant women, and people with disabilities. The program is administered by the Florida Department of Health and Human Services.
The MMAP program covers a wide range of health care services, including primary and preventive care, hospitalization, mental health and substance abuse services, prescription drugs, and more. The program also provides transportation assistance to help enrollees get to and from their medical appointments.
In addition to health care coverage, the MMAP program also offers enrollees access to a 24/7 nurse hotline, discounts on fitness memberships and healthy food options, and helpful resources to manage their health.
How can I enroll in the program?
If you think you or your family might be eligible for Medicaid coverage in Florida, the first step is to fill out an application. You can do this online at the Florida Department of Children and Families website, or you can pick up a paper application at your local county office.
If you’re not sure whether or not you qualify for Medicaid coverage, there’s a tool on the Florida Department of Children and Families website that can help you figure it out. Once you’ve submitted your application, a caseworker will contact you to set up an interview. This is usually done over the phone, but in some cases it might be done in person.
During the interview, the caseworker will ask you questions about your income, your assets, and your family situation. They’ll use this information to determine whether or not you qualify for Medicaid coverage. If you qualify, they’ll send you a packet of information about the program and how to enroll. If you don’t qualify, they’ll let you know what other options might be available to you.
What is the coverage under the program?
The Florida Medicaid Managed Medical Assistance (MMA) program provides health care coverage for low-income adults, families with children, pregnant women, the elderly and people with disabilities. MMA includes both physical and behavioral health care services.
What are the eligibility requirements for the program?
To be eligible for Medicaid in Florida, you must be a U.S. citizen or legal permanent resident, a resident of the state of Florida, and meet certain income and resource requirements. You must also be one of the following:
-Aged (65 or older)
-Blind
-Disabled
-A parent or caretaker relative of a minor child
-Pregnant
-A young adult age 19-21 who was previously in foster care
What are the managed care plans offered under the program?
The managed care plans offered under Florida Medicaid’s Managed Medical Assistance Program (MMAP) are as follows:
– Health Maintenance Organizations (HMOs)
– Preferred Provider Organizations (PPOs)
– Provider Service Networks (PSNs)
– Point of Service (POS) Plans
– physician hospital organizations (PHOs)
How do I choose a managed care plan?
There are many factors that you may want to consider when choosing a managed care plan. Some things you may want to think about include:
-What types of services does the plan cover?
-What is the plan’s network of providers?
-Is my doctor or hospital in the plan’s network?
-What are the plan’s copayments and deductibles?
-Does the plan have any special programs that I might be interested in, such as disease management or health coaching?
-What is the plan’s customer service like? Can I easily get in touch with a customer service representative when I need to?
-Does the plan have a good reputation? You can check with your friends, family, and other people you trust to see if they have any experience with the plan you’re considering.
How do I change my managed care plan?
You may change your Medicaid managed care plan one time per month. To make a change, contact your current plan to cancel your coverage effective the last day of the month. Then, contact the Medicaid Health Plan hotline at 1-877-711-3662 to enroll in a new plan. The hotline is available Monday through Friday, 8:00 a.m. to 6:00 p.m.
What are the rights and responsibilities of enrollees?
As an enrollee in Florida Medicaid’s Managed Medical Assistance (MMA) program, you have certain rights and responsibilities. You have the right to:
-Receive information about the MMA program in a language that you can understand
-Choose or change your primary care provider (PCP)
-Receive covered services without discrimination
-Get emergency services when you need them
-Appeal Medicaid’s decisions about your covered services
-Receive information about your health status, treatment options, and goals of care in a way that you can understand
You also have the responsibility to:
-Keep your Medicaid card up to date and show it when you get services
-Follow the treatment plan that you and your doctor develop together
-Make sure that someone who can make decisions for you knows about your MMA coverage and how to use it