Confidentiality for Medical Assistants
Contents [show]
It’s important for medical assistants to understand confidentiality and how to keep patient information private. This blog post covers the basics of medical confidentiality and what medical assistants need to know.
Checkout this video:
The Importance of Confidentiality for Medical Assistants
An important aspect of the medical assistant’s job is maintaining confidentiality. This means that any information about a patient’s health that is shared with the medical assistant must be kept private. Although it may seem like a simple task, maintaining confidentiality is not always easy. There are many opportunities for medical assistants to accidentally or inadvertently share patient information, which could lead to serious consequences.
When working with patients, medical assistants must be careful to only collect and record the information that is absolutely necessary. Any unnecessary information should be destroyed immediately. Medical assistants should also be aware of who has access to patient records and take steps to prevent unauthorized access.
Medical assistants must also be careful about what they say about patients in public or in front of other staff members. Even discussing a minor health concern in front of another person could violate confidentiality. If a medical assistant needs to discuss a patient’s case with another staff member, he or she should do so in a private area where no one else can overhear the conversation.
If a medical assistant inadvertently discloses confidential information, he or she should take immediate steps to correct the situation. For example, if a medical assistant accidentally sends an email containing confidential information to the wrong person, he or she should contact the recipient and ask them to delete the email and not share it with anyone else. If a breach of confidentiality has occurred, the medical assistant should report it to his or her supervisor so that appropriate steps can be taken to prevent it from happening again in the future.
Maintaining Patient Confidentiality
As a medical assistant, you will have access to patients’ confidential information. Maintaining the confidentiality of this information is crucial to protecting patients’ privacy and earning their trust.
There are many ways to maintain confidentiality, but some of the most important are to:
– Keep patient information secure
– Use discretion when discussing patients
– Respect patients’ right to privacy
By taking measures to protect patients’ confidential information, you can help create a safe and trusting environment for both patients and staff.
The Consequences of Violating Patient Confidentiality
Patient confidentiality is an important aspect of the doctor-patient relationship. It is the legal right of patients to have their medical information kept private. This right is not absolute, however, and there are circumstances in which confidentiality may be breached without the patient’s consent. In some cases, such a breach may be justified, while in others it may be considered a violation of the patient’s rights.
The consequences of violating patient confidentiality can be serious. Doctors who breach confidentiality may face disciplinary action from their employers or licensing boards. They may also be subject to civil or criminal penalties. Patients who have had their confidential information disclosed without their consent may sue for damages.
When deciding whether to disclose confidential information, doctors must weigh the interests of their patients against other competing interests. In some cases, such as when a patient is at risk of harming themselves or others, the interests of public safety may outweigh the need for confidentiality. In other cases, disclosure may be justified if it is necessary to protect the doctor-patient relationship or to ensure the quality of medical care.
How to Maintain Patient Confidentiality
As a medical assistant, you will have access to patients’ protected health information (PHI). The health insurance Portability and Accountability Act (HIPAA) is a federal law that requires all healthcare providers to maintain the confidentiality of PHI. Here are some tips to help you protect your patients’ PHI:
-Don’t discuss patients outside of work. This includes friends, family, and even other patients.
-Don’t leave patient information where others can see it. This includes computer screens, desks, and filing cabinets.
-Don’t access patient records unless you have a legitimate reason to do so.
-Keep patient information confidential even after they leave your care.
-If you see or hear something that violates HIPAA, report it to your supervisor immediately.
The HIPAA Privacy Rule
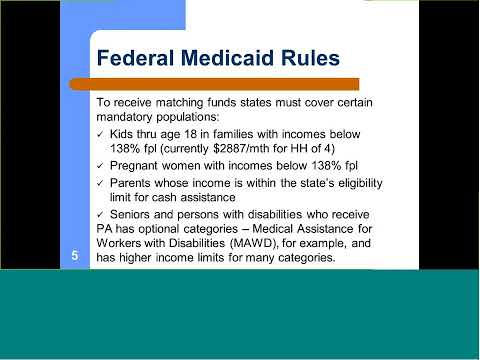
The health insurance Portability and Accountability Act (HIPAA) of 1996 established national standards to protect individuals’ medical records and other personal health information. The Privacy Rule, which was created as part of HIPAA, establishes standards for the protection of this information. The Rule requires covered entities – which include healthcare providers, healthcare clearinghouses, and health plans – to take measures to ensure the confidentiality of protected health information (PHI).
The Privacy Rule gives patients the right to access their own Medical records the right to request restrictions on how their PHI is used or disclosed, and the right to request that their PHI be communicated to them in a confidential manner. Patients also have the right to file a complaint if they believe their privacy rights have been violated.
Covered entities are required by the Privacy Rule to maintain a record of disclosures of PHI. They must also provide patients with a notice of their privacy practices. Patients have the right to request a copy of this notice.
The Privacy Rule does not apply to information that is collected by individuals who are not covered entities – for example, employers or life insurance companies. However, other federal and state laws may provide privacy protections for this type of information.
The HIPAA Security Rule
The HIPAA Security Rule applies to all forms of protected health information (PHI), whether electronic, written, or oral. The Rule establishes national standards to protect individuals’ medical records and other personal health information and applies to all forms of PHI, including:
-Medical records and other health information created or received by healthcare providers, such as hospitals, clinics, or physician’s offices
-Health plans, such as insurance companies, HMOs, and business associate contracts
-Clearinghouses that process or translate PHI from one format to another
In order to comply with the Rule, covered entities must take reasonable steps to protect the confidentiality of PHI. This includes ensuring that only authorized personnel have access to PHI and that PHI is not disclosed to unauthorized individuals. Covered entities must also take steps to ensure that PHI is accurate and secure.
The HIPAA Security Rule is divided into three main sections:
-Administrative Safeguards: These are administrative policies and procedures designed to protect the confidentiality of PHI. Administrative safeguards include measures such as developing security awareness training programs and security incident response plans.
-Physical Safeguards: These are physical security measures designed to protect against unauthorized access to PHI. Physical safeguards include measures such as locked cabinets and restricted access areas.
-Technical Safeguards: These are technical security measures designed to protect against unauthorized access to PHI. Technical safeguards include measures such as encryption and firewalls.
The HITECH Act
The HITECH Act, which was passed as part of the American Recovery and Reinvestment Act of 2009, gives patients more control over their health information and makes it easier for them to get access to it. It also imposes new privacy and security rules on healthcare providers and gives the government new powers to enforce those rules.
The HITECH Act requires healthcare providers to give patients a notice of their privacy rights, including the right to request restrictions on how their health information is used and disclosed. Healthcare providers must also take steps to secure patients’ health information from unauthorized access, use, or disclosure.
The HITECH Act gives the government new enforcement powers, including the right to impose civil and criminal penalties on healthcare providers who violate the law. The Department of Health and Human Services (HHS) is responsible for enforcing the HITECH Act, and it has set up a website with information about the law and how it will be enforced.
The Patient Bill of Rights
The Patient Bill of Rights is a set of ethical principles thathealthcare providers must adhere to in order to ensure that their patients receive the highest quality of care possible. These principles include the right to privacy, the right to informed consent, the right to refuse treatment, and the right to access medical records.
The health insurance Portability and Accountability Act
The health insurance Portability and Accountability Act (HIPAA) is a law that was passed in 1996 to protect the confidentiality of a patient’s medical information. As a medical assistant, you will have access to confidential information about your patients and it is important that you understand the rules of HIPAA.
All medical assistants must receive training on HIPAA and must sign a confidentiality agreement before they begin working. This agreement states that they will not share any confidential information with anyone who is not authorized to see it.
If you have any questions about HIPAA or how to handle confidential information, you should ask your supervisor or the office manager. They will be able to provide you with more information and help you to understand the rules.
The Family Educational Rights and Privacy Act
The Family Educational Rights and Privacy Act (FERPA) of 1974 is a federal law that protects the confidentiality of student education records. The law applies to all educational institutions that receive funding from the U.S. Department of Education. Medical Assistants should be aware of FERPA as it applies to their work in healthcare settings.
FERPA gives students the right to inspect and review their educational records, the right to request changes to inaccurate or misleading information in their records, and the right to restrict disclosure of information from their records. Under FERPA, medical assistants are considered “school officials” and may access student records without the student’s consent if it is determined that access is “in the best interest of the student.”
However, there are some exceptions to FERPA protections. For example, medical assistants may disclose information from student education records without consent if the disclosure is made:
-To school officials with a legitimate educational interest in the information
-To parents or legal guardians of a student who is a dependent for tax purposes
-In response to a court order or subpoena
-In an emergency situation where the health or safety of a student is at risk