CLIA Regulations Prohibit the Medical Assistant from Performing These Tasks
Contents [show]
CLIA Regulations Prohibit the medical assistant from Performing These Tasks. If you are a medical assistant it is important to know which tasks you are and are not allowed to perform.
Checkout this video:
CLIA Regulations
There are many things that a medical assistant is not allowed to do in the lab. This is regulated by the Clinical Laboratory Improvement Amendments (CLIA). CLIA sets quality standards for all laboratory testing to ensure the accuracy and reliability of patient test results, regardless of where the testing is performed.
There are three main areas where MA’s are prohibited from working:
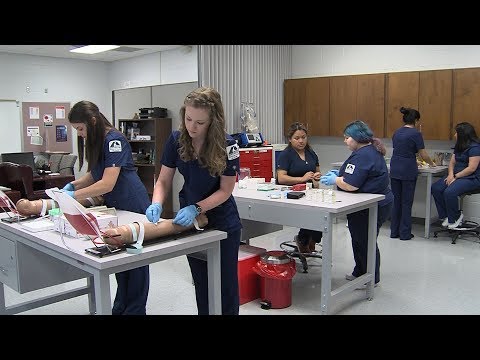
1) specimen collection- this includes venipuncture, urine collection, and capillary sticks
2) processing specimens- this includes centrifugation, serration, and dilution
3) result reporting- this includes writing results in the medical record or calling them to the physician/provider
Prohibited Tasks
The CLIA (Clinical Laboratory Improvement Amendments) regulations contain a list of 51 moderate and high complexity tests that may only be performed by laboratory personnel who meet specific education and training requirements. These tests are divided into two categories: waived and non-waived.
The following tasks are prohibited for Medical assistants
– Collection of blood specimens from arterial or venous sites
– Performance of skin puncture to collect blood specimens
– Analysis of specimens for the purpose of diagnosis or treatment
—
CLIA and the Medical Assistant
The Clinical Laboratory Improvement Amendments (CLIA) of 1988 are federal regulations that apply to all laboratory testing performed on humans in the United States regardless of complexity. The regulations are designed to ensure the accuracy, precision, and reliability of test results regardless of where the testing is performed.
To be in compliance with CLIA regulations, laboratories must be accredited by an authorized accrediting organization. Laboratories that perform only waived tests or who meet specific criteria may be exempt from accreditation.
Medical assistants cannot perform tasks that fall under the regulatory scope of CLIA. These tasks are referred to as “moderate and high complexity” and can only be performed by individuals who have met specific training and education requirements and have passed a national examination.
The following is a list of tasks that Medical Assistants cannot perform under CLIA regulations:
-Drawing and collecting blood samples from patients
-Preparing blood samples for testing
-Running tests on blood samples
-Interpreting test results
The Importance of Following CLIA Regulations
As a medical assistant it is important that you are aware of the Clinical Laboratory Improvement Amendments (CLIA) and follow the regulations set forth by this organization. CLIA is a quality control program that establishes standards for all clinical laboratories in the United States. The program is overseen by the Centers for Medicare and Medicaid Services (CMS).
One of the key aspects of CLIA is to ensure that laboratories are performing testing correctly and producing accurate results. To do this, CLIA puts restrictions on who can perform certain tasks in the laboratory. For example, only individuals who have been properly trained and have demonstrated competency can perform high-complexity testing.
Medical assistants are not allowed to perform any tasks that are considered high-complexity under CLIA regulations. This includes tasks such as operating certain types of laboratory equipment, performing certain types of testing, and interpreting test results. In some cases, medical assistants may be allowed to assist with these tasks under the supervision of a qualified laboratory professional.
It is important to be familiar with CLIA regulations and understand which tasks you are and are not allowed to perform in the laboratory. This will help ensure that you are providing quality patient care and not putting patients at risk.
What Happens if CLIA Regulations are Not Followed?
If your laboratory does not follow CLIA regulations, you may be subject to civil monetary penalties (CMPs). These are fines that can be imposed by the Centers for Medicare and Medicaid Services (CMS) for non-compliance. In addition, your laboratory could be placed on probation, which would restrict your ability to bill Medicare and Medicaid for services. Finally, your CLIA certificate could be revoked, which would completely prohibit you from billing Medicare and Medicaid.
Tips for Following CLIA Regulations
The Clinical Laboratory Improvement Amendments (CLIA) were enacted in 1988 to ensure the quality of laboratory testing. These regulations apply to all facilities that perform diagnostic or preventive lab tests on humans for the purpose of providing information for the diagnosis, prevention or treatment of any disease or impairment of, or assessment of the health of, an individual.
To ensure compliance with CLIA regulations, medical assistants must be aware of which tasks they are allowed to perform and which tasks require certification. The following is a list of tasks that medical assistants are not allowed to perform under CLIA regulations:
-Drawing blood from a vein (venipuncture)
-Collecting specimens other than blood from body surfaces (e.g., skin, mucous membranes)
-Setting up equipment for procedures
-Cleaning and sterilizing equipment
-Performing quality control checks on equipment and supplies
-Calibrating or troubleshooting equipment
-Performing waived tests
CLIA Regulations and Your Practice
The Clinical Laboratory Improvement Amendments (CLIA) of 1988 are federal regulations that govern all clinical laboratory testing performed on humans in the United States, regardless of who performs the test or where it is performed.
There are three types of CLIA regulations: general requirements, personnel requirements, and quality control requirements. All three types of regulations must be met in order for a laboratory to receive a Certificate of Waiver, Certificate of Compliance, or Certificate of Accreditation.
The general requirements state that all laboratories must have a written policy manual specifying the procedures that will be used to ensure the accuracy and precision of test results. The policy manual must be approved by the laboratory director and must be available to all personnel who perform or supervise testing.
The personnel requirements state that all individuals who perform or supervise testing must have adequate training and experience in the specific test procedures being used. In addition, these individuals must be competent to perform their assigned tasks and must be able to understand and follow instructions.
The quality control requirements state that all laboratories must establish and maintain quality control procedures to ensure the accuracy and precision of test results. These procedures must be designed to detect and correct errors that may occur during the testing process. Quality control procedures must be performed on every batch of tests run by the laboratory, and records of these quality control procedures must be maintained.
CLIA Regulations and Patient Safety
The Clinical Laboratory Improvement Amendments (CLIA) were enacted in 1988 to ensure the quality of clinical laboratory testing. These regulations establish standards for all US facilities that perform medical laboratory testing, regardless of whether the test results are used for diagnosis, prevention, or treatment.
All medical laboratories must be certified by CLIA in order to operate. Certification is granted by the Centers for Medicare and Medicaid Services (CMS), and it is dependent on meeting certain standards. Laboratories can be accredited by private organizations, but this is not required by CLIA.
The CLIA regulations are extensive, and they cover everything from personnel qualifications to test methodology. One of the key provisions of CLIA is that it prohibits non-laboratory personnel from performing certain tasks that could potentially jeopardize patient safety.
Medical assistants are not allowed to perform any tasks that are considered to be high-complexity under CLIA. This includes any tasks that have the potential to cause “an adverse event” in the patient. Adverse events can include errors in test results, false positives, false negatives, and even death.
Some of the high-complexity tasks that medical assistants are not allowed to perform include:
-Drawing blood from a vein (venipuncture)
-Performing skin punctures for blood collection
-Operating complex lab equipment
-Performing lab tests that require special training (e.g., pap smears)
CLIA Regulations and Quality of Care
The Clinical Laboratory Improvement Amendments (CLIA) of 1988 are United States federal regulatory standards that apply to all clinical laboratories. The regulations are meant to ensure the accuracy and precision of laboratory tests performed on human specimens for the diagnosis, prevention or treatment of any disease.
There are three categories of regulated tasks: waived, moderate and high complexity. Waived tests are simple, routine tests that have a very low likelihood of producing an erroneous result. Moderate complexity tests are those that require more attention to detail and greater procedural knowledge, but still have a relatively low chance of producing an erroneous result. High complexity tests are those with a relatively high chance of producing an erroneous result, and require a greater degree of skill and training to perform correctly.
The CLIA regulations prohibit medical assistants from performing any tasks that fall into the moderate or high complexity categories. This means that medical assistants cannot perform most laboratory testing, including blood work and urine analysis.
While this may seem like a hindrance to providing quality patient care, there are actually several reasons why the CLIA regulations are in place. First, waived tests are typically used for screening purposes only, so it is important that they be as accurate as possible. Second, moderate and high complexity tests can provide critical information about a patient’s health status, so it is important that they be performed correctly in order to avoid misdiagnosis or delayed diagnosis. Finally, performing these types of tests requiresspecific training and experience that medical assistants typically do not possess.
In summary, the CLIA regulations exist to protect patients by ensuring that laboratory testing is performed accurately and precisely. Medical assistants cannot perform most laboratory testing because it requires specific training and experience that they typically do not possess.
Resources for Following CLIA Regulations
The Clinical Laboratory Improvement Amendments (CLIA) were enacted in 1988 to ensure the accuracy and quality of laboratory testing. Since then, the Centers for Medicare and Medicaid Services (CMS) has been responsible for enforcing CLIA regulations.
The Maternal and Child Health Bureau (MCHB) also provides federal oversight of state-based newborn screening programs. Newborn screening tests are performed on all babies born in the United States to look for evidence of more than 30 serious conditions that can affect a baby’s health.
CLIA covers all US FDA-regulated laboratories that perform clinical tests on humans for the purposes of providing information for diagnosis, prevention, or treatment of any disease or assessment of health. This includes CLIA-waived tests, which are simple tests that pose no risk if performed incorrectly.