Which of the Following is Not a Principle of a Patient-centered Medical Home Practice?
Contents [show]
A Medical Home is a model of care that focuses on the patient’s needs and preferences. The goal of a medical home is to create a partnership between patients, providers, and community resources.
The the predominant services of local public health departments today are: is not a principle of a patient-centered medical home practice.
This Video Should Help:
What is a Patient-centered Medical Home Practice?
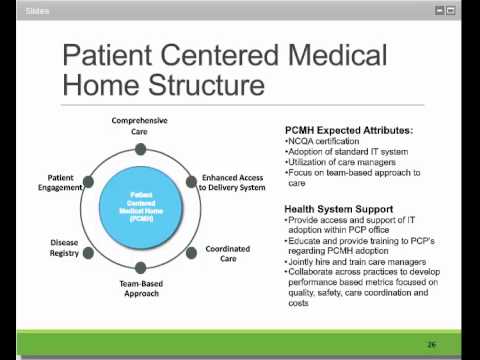
The concept of a patient-centered medical home (PCMH) practice is gaining popularity as a model for primary care delivery. The PCMH is a health care delivery model that emphasizes comprehensive, continuous, and coordinated care delivered in a manner that is patient-centered, family-oriented, and community-based. A growing body of evidence suggests that the PCMH can improve quality of care and patient satisfaction while reducing costs.
There is no single definition of the PCMH, but there are several key principles that are typically included:
1. A focus on preventive care and health promotion
2. Comprehensive and continuous care
3. Coordinated care among providers
4. Patient-centered care
5. Use of health information technology
6. A team-based approach to care delivery
7. A focus on population health management
What are the Principles of a Patient-centered Medical Home Practice?
1. The discussion of the principles of a patient-centered medical home delivery model begins with acknowledgments of the framework within which the delivery model functions.
2. The delivery model should promote preventive services and address chronic disease management needs.
3. Patients should be active participants in their health care, with education and support provided by the care team to facilitate this engagement.
4. The medical home should be accessible, using various modalities including but not limited to extended office hours, same-day appointments, and proactive follow-up after discharge from the hospital or emergency department.
5. Care should be coordinated across all providers involved in a patientufffds care, including specialists, home health care agencies, and other ancillary services.
6. The medical home should use data to drive quality improvement initiatives with the goal of continuously improving patient outcomes.
7. The delivery model should be designed to meet the specific needs of each individual patient population served by the practice.
8. Payment reform should incentivize attainment of improved clinical outcomes while reducing costs associated with unnecessary tests and procedures.
Which of the Following is Not a Principle of a Patient-centered Medical Home Practice?
There is much discussion about the role of the medical home in improving patient care and preventing illness. The following principles are generally accepted as key components of a patient-centered medical home practice:
1. Accessibility: Proactive, continuous, comprehensive care is readily available to all who need it.
2. Appropriateness: Care is provided in the most effective setting and promotes patients’ safety and quality of life.
3. Continuity: Care is coordinated and integrated across all levels of the health care system.
4. Efficiency: Care is delivered in a cost-effective manner.
5. Effectiveness: Care is based on best evidence and meets patients’ health needs.
6. Patient-centeredness: Care is tailored to meet the unique needs and preferences of each patient.
7. Quality and safety: Care is safe and meets high quality standards.
8. Teamwork: Care is delivered by a team of providers who work together to meet patients’ needs.
9.. Cultural competence: Care takes into account patients’ cultural beliefs and practices.
10.. Privacy and confidentiality : Patients’ health information is private and confidential .
What are the Benefits of a Patient-centered Medical Home Practice?
The patient-centered medical home is a model of care that puts patients at the center of their care. This model of care is based on four key principles:
1. Patient-centered: The patient is at the center of all decisions made about their care.
2. Comprehensive: All aspects of a patient’s care are considered when making decisions about their care.
3. Coordinated: Care is coordinated across all providers and Settings to ensure that patients receive the best possible care.
4. Accessible: Patients have access to the care they need, when they need it.
How can I Implement a Patient-centered Medical Home Practice?
There is no single blueprint for a patient-centered medical home (PCMH) practice, but there are certain key principles that all practices should aim to implement. These include:
-Discussion and shared decision-making between patients and clinicians
-A focus on preventive care and health promotion
-The use of evidence-based guidelines to inform clinical decision-making
-The tracking and monitoring of patientsufffd health outcomes
-Regular feedback and review of clinical results with patients
Some other important considerations for setting up a PCMH practice include:
– Adequate staffing levels, including a mix of clinicians with different skills and training
– The use of information technology to support clinical decision-making, patient engagement, and care coordination
– The incorporation of patient perspectives into quality improvement initiatives.
What are the Challenges of a Patient-centered Medical Home Practice?
There is much discussion in the medical community about whether the patient-centered medical home model of delivery is the best way to provide preventive services and produce the best results. The main challenges of a patient-centered medical home practice are:
-Javascript must be enabled to use this site.
-Adequate staffing levels, especially of nurses and social workers;
-The need for strong Electronic health records (EHR) and other technology infrastructure;
-Engaging patients and their families in care;
-Finding ways to measure and report outcomes;
-Ensuring continuity of care when patients see other providers outside the practice.
What is the Future of Patient-centered Medical Home Practices?
The patient-centered medical home is a model of care that delivers coordinated care through a partnership between patients and their providers. The goal of this care delivery model is to improve patient outcomes by providing preventive services, coordinating care among different specialists, and involving patients in their own care.
In a recent survey of patient-centered medical home practices, 62 percent of respondents said they were very likely to continue operating as a medical home, and another 28 percent said they were somewhat likely to continue operating as a medical home. These results suggest that patient-centered medical homes are here to stay and that they are likely to continue to grow in popularity in the years to come.
There are several reasons why patient-centered medical homes are becoming more popular. First, they have been shown to improve patient outcomes. A recent study found that patients who receive care from a medical home are more likely to receive preventive services and have better self-reported health status than those who do not receive care from a medical home.
Second, patient-centered medical homes can save money. A recent study found that patients who receive care from a medical home cost $2,564 less per year than those who do not receive care from a medical home. This savings is due to the fact that patients who receive care from a medical home are less likely to use emergency services, be hospitalized, or require long-term care.
Finally, patient-centered medical homes improve provider satisfaction. In the same survey mentioned above, providers who worked in a patient-centeredmedical home were more likely to report high job satisfaction than those who did not work in a patient-centeredmedical home. This is likely due to the fact that providers who work in a patient-centeredmedical home have more time to spend with their patients and are less likely to experience burnout.
Case Study: Implementing a Patient-centered Medical Home Practice
Discussion
The objective of this case study was to explore the potential of a patient-centered medical home (PCMH) practice model in which registered nurses (RNs) proactively coordinate care for patients with chronic conditions. The study employed a multicase design with data collected from five clinics across the United States Data sources included field observations, interviews with key informants, and document reviews.
Preventive services were identified as a primary driver of improved clinical outcomes and cost savings in the PCMH model. However, implementation challenges related to provider resistance, front-office staff buy-in, and IT infrastructure support were also noted. Overall, the results of this study suggest that a PCMH practice model is feasible and has the potential to improve clinical outcomes and reduce costs associated with care for patients with chronic conditions.
Acknowledgments
The authors would like to acknowledge the following individuals for their contributions to this case study:
-Javascript must be enabled to view this email address] for her technical expertise and support throughout the project;
-The home care RNs who participated in this study;
-The patients who graciously shared their stories;
-And finally, the senior leadership at each site who provided unwavering support for this effort.
FAQs about Patient-centered Medical Home Practices
The following are principles of a Patient-centered Medical Home Practice:
-Delivery of preventive services with an emphasis on health Promotion and Disease Prevention
-Discussion of test results and treatment options with patients and caregivers
-Use of evidence basedpractice guidelines
-Coordination and communication among all members of the patient’s care team
-Javascript must be enabled to use this site.
Further Reading on Patient-centered Medical Home Practices
The Patient-centered Medical Home is an approach to primary care that puts patients at the center of their own care. This means that patients are actively involved in decisions about their own health, and that their physicians work with them to develop a plan of care that is tailored to their individual needs.
There are several principles that have been identified as key to successful implementation of a Patient-centered Medical Home:
-Discussion: Patients and their families should be included in discussions about their care, and should be given the opportunity to ask questions and express their preferences.
-Preventive services: Patients should be offered preventive services that are tailored to their individual needs, and they should be given the opportunity to discuss their risks for specific conditions.
-Results: Patients should be given access to their own medical records, so that they can track their progress and see the results of any tests or procedures.
-Acknowledgments: Patients should be acknowledged as part of the team, and should feel comfortable communicating with their physicians about their care.
The “to provide direct patient care, physicians are required to do all of the following except:” is not a principle of a Patient-centered Medical Home Practice. The other three principles are:
1) To establish an effective referral relationship with patients; 2) To coordinate care among providers; 3) To provide quality care
External References-
https://quizlet.com/229516447/3111-chapter-5-flash-cards/
https://quizlet.com/54646381/the-patient-centered-medical-home-oct-13-flash-cards/
https://quizlet.com/183271950/patient-centered-medical-homes-flash-cards/