Medical Home Affordable Care Act
Contents [show]
The Affordable Care Act is a law that was passed by the US Congress in 2010 to provide Affordable Health Care for all Americans. It has been the subject of much debate and controversy, but its effects have been felt throughout the country. Now, with the Trump Administration in power, it remains uncertain what will happen to this landmark legislation.
The Affordable Health Care Act is a law that was passed in 2010. The bill expanded health care coverage for Americans by mandating that all individuals have access to affordable health insurance and by prohibiting insurance companies from denying coverage based on pre-existing conditions.
This Video Should Help:
The Medical Home and the Affordable Care Act
Under the Patient Protection and Affordable Care Act (ACA), all Americans will be required to have health insurance starting in 2014. The ACA puts in place a number of reforms that will affect how people get health care and how much they pay for it. One of these reforms is the creation of the medical home.
The medical home is a model of care that puts the patient at the center of his or her own care. The medical home is a team-based approach to health care, with the team working together to coordinate all of the patient’s care needs. The Affordable Care Act includes a number of provisions to promote the use of the medical home model, including:
-Allowing primary care physicians to form Patient-Centered Medical Homes (PCMHs), which are teams of providers that work together to coordinate all of a patient’s care needs;
-Providing Americans with easier access to primary care and preventive services by expanding Medicaid coverage and increasing funding for Community Health Centers;
-Giving states flexibility to create their own Medicaid programs that promote the use of medical homes; and
-Creating incentives for physicians to become part of PCMHs.
The medical home model of care
The Patient Protection and Affordable Care Act (ACA) requires, as a condition of receiving federal funding, that state Medicaid programs implement the medical home model of care delivery by 2015. Also known as the “health home” model, this coordinated care delivery approach has been shown to improve health outcomes and to reduce costs, especially for patients with chronic diseases. Under the ACA, a “medical home” is defined as a health care setting that (1) provides comprehensive primary care services, (2) coordinates and integrates all necessary health and social services for individuals and families who are enrolled in the state Medicaid program (“Enrollees”), and (3) ensures that each Enrollee has an ongoing relationship with a personal physician or nurse practitioner who provides comprehensive primary care services and coordinates all aspects of the Enrollee’s health care.
In order to receive federal funding, state Medicaid programs must implement the medical home model of care delivery by 2015. The Patient Protection and Affordable Care Act (“ACA”) requires that all state Medicaid programs implement this coordinated care delivery approach in order to receive federal funding. The medical home model of care delivery has been shown to improve health outcomes while also reducing costs, making it an attractive choice for states seeking to improve their Medicaid programs.
The benefits of the medical home model
The medical home model of health care delivery is gaining popularity and support from both the public and the private sectors. The medical home is a concept that shifts the focus of care from sick-care to health promotion and disease prevention. The goal of the medical home is to provide high-quality, coordinated, patient-centered care.
There are many benefits of the medical home model of health care delivery, including:
– improved health outcomes for patients
– better coordination of care
– improved communication between patients and providers
– increased patient satisfaction
– lower costs of care
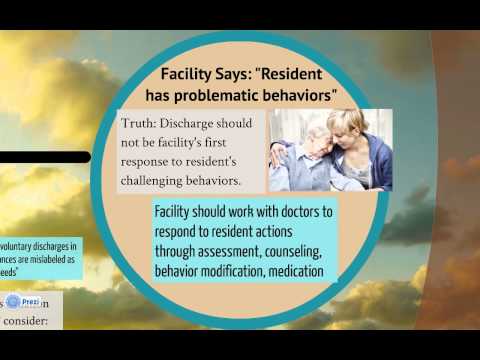
The challenges of the medical home model
One of the challenges of the medical home model is that it requires a certain amount of coordination and communication between the primary care provider (PCP), specialists, and other members of the care team. This can be a challenge for practices that are used to working independently. In addition, the medical home model requires practices to track a number of quality measures and patient-centered medical home (PCMH) standards. These quality measures can be time-consuming to track and report on, and may require practices to invest in new health information technology (HIT) systems.
The medical home and chronic disease management
The medical home is a key concept in the Affordable Care Act (ACA). The ACAufffds Patient-centered medical home (PCMH) model of care delivery is built around the idea that better health outcomes can be achieved, and health care costs can be controlled, when patients receive coordinated, continuous, and comprehensive care from a team of providers who know them well.
chronically ill patients account for a large share of the nationufffds health care costsufffdan estimated 75 percent.
The ACA established the CMS Innovation Center to test new models of care delivery that have the potential to improve quality and lower costs. One such model is the PCMH.
The PCMH is a model of care that emphasizes communication and coordination among all members of a patientufffds health care team. The goal is to provide each patient with continuous, comprehensive care that is coordinated and integrated across all segments of the health care system.
A key feature of the PCMH is that it gives primary care providers (PCPs) financial incentives to coordinate the care their patients receive from specialists, hospitals, and other health care professionals. In addition, PCPs are held accountable for ensuring that their patients receive preventive services and necessary follow-up care after they leave the hospital or an outpatient facility.
###HHS on Patient-Centered Medical Homes: ufffdA patient-centered medical home is not a building, house, or office. It may be any site where primary care services are delivered, including physician practices, clinics, community health centers, hospitals, or even schools-based health centersufffd The fundamental components of a patient-centered medical home include: Accessible location; extended hoursufffdComprehensive services including behavioral healthufffd A team based approach; Electronic Health Records; Coordination with other providers; engages patients/families as partners in their own healthcare . . . You will know you are in a medical home if your provider: Spends time getting to know you as a person; Helps you make choices about your healthcare; Follows up with you after you have been seen in the office or hospital; Calls you between visits if he or she thinks you need extra supportufffd Makes sure other providers involved in your care have the information they need so everyone works together for your benefit.”
The medical home and preventive care
The medical home is a model of care that puts the patient at the center of their care team. It aims to improve health outcomes and quality of life by providing coordinated, patient-centered care. The medical home model has been shown to improve health outcomes, reduce costs, and increase patient satisfaction.
The Affordable Care Act (ACA) promotes the use of the medical home model by giving primary care providers financial incentives to provide coordinated, patient-centered care. Under the ACA, providers who meet certain criteria can receive extra payments for providing preventive services and coordinating care.
The ACA also requires all new private health plans to cover a set of preventive services without charging a copayment or coinsurance. These services include screenings for blood pressure, cholesterol, diabetes, and cancer, as well as vaccinations for influenza and pneumonia.
The medical home and patient engagement
The Patient Protection and Affordable Care Act (ACA) contains a number of provisions that are designed to encourage patients to take a more active role in their health care (i.e., patient engagement). One of these provisions is the creation of medical homes. A medical home is a health care delivery model that emphasizes care coordination and communication among a patientufffds various health care providers, with the goal of providing comprehensive, well-coordinated, patient-centered care. Under the ACA, providers who establish medical homes can receive enhanced payments from Medicare and Medicaid.
There are a number of different models for medical homes, but they all share certain key features, including:
-A designated provider or team of providers that coordinates all aspects of a patientufffds care;
-A focus on preventive care and health promotion;
-An emphasis on coordinated care among a patientufffds various health care providers;
-Extended hours and easy access to care;
-A focus on patients as partners in their own care; and
-The use of information technology to support the delivery of care.
The medical home and care coordination
The medical home is an approach to providing comprehensive primary care that is patient-centered, continuous, coordinated, accessible, and focused on quality and safety. The goal of the medical home is to improve health outcomes and to achieve a better patient experience of care while reducing costs.
The Affordable Care Act (ACA) requires that HHS develop and implement a national strategy to promote care coordination and the medical home model of care delivery. To this end, HHS has established five key points of focus for the national strategy:
– Establishing payment models that incentivize care coordination and the delivery of high-quality, patient-centered care;
– Encouraging the use of health information technology (HIT) to support care coordination;
– Promoting workforce development for the delivery of coordinated, patient-centered care;
– Increasing investment in evidence-based programs that support care coordination; and
– Fostering innovation in research on new models of care delivery.
The medical home and population health
The Patient Protection and Affordable Care Act (ufffdPPACAufffd) was signed into law by President Barack Obama on March 23, 2010. Among other things, PPACA establishes a new ufffdmedical homeufffd delivery model for primary care and requires all insurers to offer coverage for preventive services without any patient cost-sharing.
A ufffdmedical homeufffd is a model of care that provides comprehensive, continuous, coordinated, family-centered, compassionate care. The medical home is not a place, but rather a team-based model of care led by a primary care provider who coordinates all of the patientufffds health care needs.
The goal of the medical home delivery model is to improve health outcomes and reduce costs by providing high-quality, coordinated care that is patient-centered and focused on prevention. In order to achieve these goals, medical homes must be held accountable for their performance on a set of quality measures. The Centers for Medicare & Medicaid Services (CMS) has established 10 core measures that all medical homes must report on:
1) Access to care ufffd appointments within 2 weeks
2) Preventive care ufffd screenings and vaccinations up to date
3) continuity of care ufffd seeing the same doctor for recurring visits
4) after-hours access ufffd 24/7 advice line or email/secure messaging with doctor
5) coordination of care ufffd specialists know about your condition and treatment plan
6) patient education ufffd know what your diagnosis means and what treatments are available
7) self-management support ufffd help making lifestyle changes or managing chronic disease
8) transitions in care ufffd following up after leaving the hospital or going to a specialist
9) use of health information technology ufffd able to view test results and securely message doctors
10) tracking clinical measures ufffd such as blood pressure or cholesterol levels
The future of the medical home
As we enter into a new decade, the Affordable Care Act (ACA) will continue to shape the delivery of health care in the United States The medical home model of care, which is centered on building relationships between patients and their primary care providers, is one of the ACAufffds key strategies for improving quality and reducing costs.
There are several reasons why the medical home model is well-suited to meeting the needs of patients in the ACA era. First, medical homes place a strong emphasis on preventive care, which can help to avert costly and avoidable health problems before they start. Second, medical homes promote continuity of care by encouraging patients to see the same provider for all of their health care needs. This continuity of care helps to ensure that patients receive timely and coordinated services, and that their providers have a complete picture of their health history.
Third, medical homes use a team-based approach to care, which allows providers to draw on the expertise of other members of the team when treating patients. This team-based approach helps to improve communication among providers and reduces duplication of services. Fourth, medical homes make use of health information technology (HIT), which can help providers to more effectively manage patientsufffd health information and make better informed decisions about their care. Finally, medical homes focus on quality improvement, which helps to ensure that providers are continually striving to improve the quality and efficiency of care.
The ACAufffds medical home provisions are designed to encourage more widespread adoption of the medical home model by providing incentives for providers who achieve certain performance milestones. The ACA also provides funding for HIT infrastructure and training programs that will help provider organizations implement medical homes within their practices. In addition, the ACA establishes new quality reporting requirements for provider organizations that participate in Medicare and Medicaid, which will help to drive quality improvement efforts within these organizations.
Looking ahead, it is clear that the medical home model of care will play a central role in shaping the future of health care in America. The ACAufffds incentives and investments will help to ensure that more Americans have access to high-quality, coordinated, patient-centered care.
The “how did the affordable care act fail to provide access to healthcare for all individuals?” is a question that has been asked many times. The Affordable Care Act was supposed to provide health care for all, but it failed in its mission.