What Medical Assistants Need to Know about Coding and Billing
Contents
- What is coding and billing?
- What do medical assistants need to know about coding?
- What do medical assistants need to know about billing?
- How can medical assistants use coding to improve patient care?
- How can medical assistants use billing to improve patient care?
- What coding and billing resources are available to medical assistants?
- How can medical assistants stay up-to-date on coding and billing changes?
- What coding and billing challenges do medical assistants face?
- How can medical assistants overcome coding and billing challenges?
- What are the future trends in coding and billing?
Medical Assistants need to know about coding and billing in order to perform their job duties correctly. This blog post will cover what Medical assistants need to know about coding and billing.
Checkout this video:
What is coding and billing?
Coding and billing is the process of translating medical procedures and diagnoses into code numbers that are then used to generate patient bills. This process is essential to the proper functioning of the healthcare system, as it ensures that providers are properly reimbursed for their services and that patients are only billed for the care they receive.
Medical assistants need to have a basic understanding of coding and billing in order to perform their job duties effectively. They may be responsible for entering patient information into coding and billing software, reviewing patient bills for accuracy, or assisting patients with questions about their bill. It is also important for medical assistants to be familiar with common coding and billing terms, so that they can communicate effectively with other members of the healthcare team.
What do medical assistants need to know about coding?
As the medical field increasingly relies on technology, medical assistants must be proficient in coding in order to help maintain accurate patient records. Similarly, an understanding of billing and insurance processes is necessary to help keep the office running smoothly. Here’s what you need to know about coding and billing as a medical assistant
Coding is the process of assigning numerical codes to diagnoses and treatments in order to track patient care and generate billing claims. In order to code effectively, medical assistants must be able to interpret doctors’ notes and understand Medical Terminology There are many different coding systems in use, so it’s important to be familiar with the most common ones, such as the International Classification of Diseases (ICD) and the Current Procedural Terminology (CPT).
Billing is the process of submitting claims to insurance companies for reimbursement. In order to bill correctly, medical assistants must be aware of the different types of insurance plans and understand how each one works. They must also be familiar with coding in order to properly submit claims. Claims can be submitted electronically or by paper, depending on the insurance company’s requirements.
Coding and billing are complex processes, but they are essential for keeping the office running smoothly. Medical assistants who are proficient in these areas will be able to provide a valuable service to their patients and their employer.
What do medical assistants need to know about billing?
Coding and billing is a process whereby medical assistants convert the services rendered by physicians and other health care providers into numeric or alphanumeric codes. These codes are then used to generate claims which are submitted to insurance companies in order to receive payment for services rendered.
Medical assistants need to have a working knowledge of coding and billing in order to perform their job duties effectively. In addition, many medical assistants also possess certification in Medical coding and/or billing, which is evidence of their expertise in this area.
How can medical assistants use coding to improve patient care?
When it comes to coding and billing, medical assistants can play a key role in ensuring that patients receive the best possible care. By understanding how coding works, they can help to ensure that the right codes are used for each patient’s condition. This can in turn help to ensure that patients are properly reimbursed for their care.
In addition, medical assistants can use their knowledge of coding to help patients understand their rights and options when it comes to billing. By being able to explain the different types of codes and how they are used, medical assistants can help patients make informed decisions about their care.
How can medical assistants use billing to improve patient care?
Medical assistants can play a vital role in improving patient care by understanding the basics of coding and billing. With this knowledge, they can help to ensure that patients receive the correct diagnosis and treatment, and that their insurance claims are processed correctly.
Coding is the process of translating diagnoses and procedures into numerical codes that are used for billing purposes. Billing is the process of submitting claims to insurance companies for reimbursement.
Understanding how coding and billing works can help medical assistants to:
-Accurately code diagnoses and procedures
-Ensure that patients receive the correct diagnosis and treatment
-File insurance claims correctly
-Obtain proper reimbursement for services rendered
-Help patients understand their medical bills
What coding and billing resources are available to medical assistants?
There are a number of resources available to medical assistants who want to learn more about coding and billing. The American Academy of Professional Coders (AAPC) offers a number of certification courses, as well as an annual coding conference. In addition, there are a number of online courses and webinars available.
How can medical assistants stay up-to-date on coding and billing changes?
In order to stay up-to-date on coding and billing changes, medical assistants should consider taking continuing education courses or subscribing to coding and billing newsletters. Additionally, they can consult with their supervisor or the office billing specialist to stay informed of any changes.
What coding and billing challenges do medical assistants face?
Coding and billing are two important functions of the medical assistant role. Medical assistants must be able to accurately code patient information in order to receive reimbursement from insurance companies. They also need to have a good understanding of the billing process in order to submit claims correctly and resolve any billing issues that may arise.
Coding can be a challenge for medical assistants because they need to have a good understanding of medical terminology and the different coding systems that are used. In addition, coding can be very time-consuming, particularly if there are a lot of codes that need to be entered.
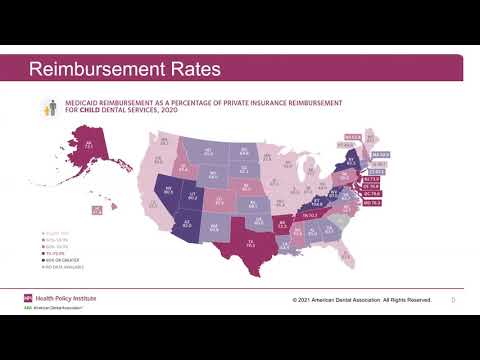
Billing can also be challenging for medical assistants. They need to have a good understanding of how insurance reimbursement works and the different types of insurance coverage that are available. In addition, billing can be very paperwork-intensive, so medical assistants need to be organized and detail-oriented in order to keep track of all the documentation that is required.
How can medical assistants overcome coding and billing challenges?
Medical assistants need to understand the basics of coding and billing in order to perform their jobs effectively. However, there are a number of challenges that can make these tasks difficult.
One challenge is that there is a lot of medical jargon involved in coding and billing. This can make it difficult to understand what the codes mean, and how to correctly apply them to patient records.
Another challenge is that coding and billing procedures are constantly changing. This can make it difficult for medical assistants to keep up with the latest information.
Finally, medical assistants may sometimes encounter resistance from physicians when they suggest changes to the way that coding and billing are conducted. Physicians may be reluctant to change their procedures, or may be unfamiliar with the latest coding and billing requirements.
Medical assistants can overcome these challenges by taking the time to learn about coding and billing, staying up-to-date on the latest information, and working closely with physicians to ensure that all procedures are followed correctly.
What are the future trends in coding and billing?
Coding and billing are integral parts of the medical office. Every day, medical assistants work with patients to obtain their health insurance information, input data into the computer, file claims, and track payments. With the ever-changing landscape of health care, it is important for medical assistants to stay current on coding and billing trends.
One of the biggest changes in coding and billing is the switch to ICD-10. ICD-10 is a more comprehensive system for classifying diseases and injuries. It went into effect in October 2015, and all medical offices were required to use it by October 1, 2016. The switch to ICD-10 has been a big adjustment for many medical offices, and there have been some growing pains. However, most offices have now made the transition and are using ICD-10 on a regular basis.
Another change that has been happening in coding and billing is the move to electronic claims submission. In the past, most claims were submitted on paper. However, more and more insurers are now requiring that claims be submitted electronically. This change has been driven by the Affordable Care Act which requires that all insurers offer electronic claim submission by January 1, 2014. Many insurers are also now offering incentive payments for providers who submit electronically.
The trend towards electronic claim submission has also led to a trend towards Electronic Health Records (EHRs). An EHR is an electronic version of a patient’s medical record. Many providers are now using EHRs instead of paper charts. EHRs offer many benefits over paper charts, including improved accuracy and efficiency. However, EHRs can also be more expensive to implement than paper charting systems.
Another trend that is happening in coding and billing is the use of new technology, such as computerized provider order entry (CPOE) systems. CPOE systems allow providers to enter orders directly into a computer instead of writing them down on paper charts. CPOE systems can improve accuracy and efficiency in the ordering process. However, they can also be expensive to implement