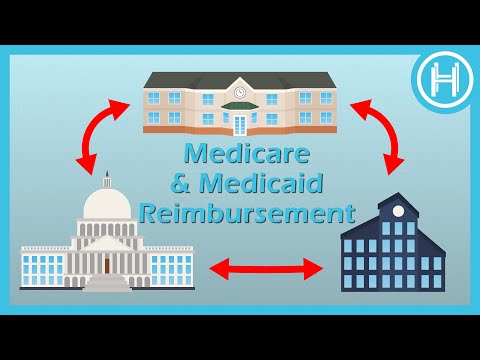
How to Get Medicaid to Reimburse Nursing Homes for Incurred Medical Expenses?
Contents [show]
You might also be thinking, Which situation would qualify an individual for receiving benefits from a qualified long term policy?
When a person is mentally challenged, a qualifying long-term care coverage must pay benefits. In which circumstances would a person be eligible to receive benefits from a qualifying long-term care policy? In this case, Home Health Care would be the best option.
Similarly, What is retroactive Medicare coverage?
You may enroll in Part A at any time after you first become eligible for Medicare if you are qualified for premium-free Part A. Your Part A coverage will begin 6 months after you join up (retroactively) (but no earlier than the first month you are eligible for Medicare).
But then this question also arises, Is medical retroactive?
Unpaid medical expenditures from three months previous to the month you apply for Medi-Cal are covered under retroactive Medi-Cal. If you have any outstanding invoices from the past three months, provide that information in your application. You will be assessed for retroactive coverage if you qualify for Medi-Cal.
What happens to your money when you go to a nursing home?
The general premise is that the nursing home receives all of your monthly income, and Medicaid reimburses the nursing home for the difference between your monthly income and the amount authorized under the nursing home’s Medicaid contract.
Does Medicaid pay for nursing home care?
Nursing Home Benefits under Medicaid If you fulfill the qualifying standards, Medicaid will cover 100% of your nursing home fees in most circumstances. The monthly income limit in most states is $2,382 for individuals and $4,764 for couples. 21.09.2021
Related Questions and Answers
Does Medicaid pay for skilled nursing facility?
Medicaid-certified nursing homes offer nursing facility services, which essentially consist of three categories of services: skilled nursing or medical care, as well as allied services. Due to an injury, disability, or sickness, rehabilitation is required.
Why is Medicare Part A retroactive 6 months?
Because she applied for Medicare and Social Security benefits more than 6 months after being first eligible, Employee’s Part A Medicare entitlement is retrospectively effective six months previous to her application for Medicare benefits (age 67 12).
Is Medicare retroactive for 6 months?
You may enroll in Part A at any time after you first become eligible for Medicare if you are qualified for premium-free Part A. Your Part A coverage will begin 6 months after you join up (retroactively) (but no earlier than the first month you are eligible for Medicare).
If you have filled any approved medications since the Retroactive Effective Date>, Medicare’s Limited Income Newly Eligible Transition (NET) Program will reimburse you for the amount you paid out of pocket, less any copayments (up to $3.70 for a generic medicine and up to $9.20 for a brand-name drug).
How does Medi-Cal reimbursement work?
Medi-Cal will send you a straight refund for the entire cost of the treatment you paid for. Reimbursement for Medi-Cal services up to the Medi-Cal rate: If Medi-Cal is unable to collect payment from the provider. 23.03.2021
How do I get Medi-Cal back pay?
Unpaid medical expenditures from three months previous to the month you apply for Medi-Cal are covered under retroactive Medi-Cal. If you have any outstanding invoices from the past three months, provide that information in your application. You will be assessed for retroactive coverage if you qualify for Medi-Cal.
How far back does Medi-Cal check your bank account?
Important note: There is a 60-month look back period for long-term care Medicaid (30-months in California). This is the time period during which Medicaid examines all previous asset transactions to verify that no assets were donated or sold for less than fair market value. 10.02.2022
How can I hide money from Medicaid?
– A trust for asset protection. Asset protection trusts are created to safeguard your assets. – Income trusts are a kind of investment trust. There is a rigorous income restriction when applying for Medicaid. Promissory notes and private annuities are two types of promissory notes. – Caregiver Contract. – Transfers for spouses.
Do all nursing homes accept Medicaid?
Medicaid may not be accepted by long-term care facilities. Medicaid payments are not accepted by all nursing homes, assisted living facilities, and other services. Whether you ask a nursing home or assisted living facility if they take Medicaid residents, they should be able to inform you.
How do I protect my assets from Medicaid in Minnesota?
In Minnesota, making a smart donation along with a Medicaid Compliant Annuity is the best method to safeguard assets.
What home health services are covered by Medicaid?
Home health services are Medicaid State Plan services offered to Medicaid users of any age on a part-time and intermittent basis. Home health nurses, home health aides, and specialized treatments are examples of home health services (physical therapy, occupational therapy, and speech-language pathology).
Does Medicaid cover assisted living?
Is assisted living covered by Medicaid? Medicaid is a sort of health insurance that covers practically all medical expenses, including some long-term care expenses. While each state has its own set of laws and restrictions, Medicaid in most states pays part of the expenses of assisted living. 01.02.2022
How much is a nursing home per month?
In 2020, the typical annual cost of nursing home care for a semi-private room was $93,075 and for a private room was $105,850. A semi-private room at a nursing home costs $7,756 per month, while a private room costs $8,821. Since 2019, the monthly cost of a semi-private room at a nursing home has climbed by 3% year over year. 30.03.2021
What is considered a skilled nursing facility?
A skilled nursing facility is an in-patient rehabilitation and medical treatment facility staffed by medical experts. Licensed nurses, physical and occupational therapists, speech pathologists, and audiologists offer medically essential treatments.
What is long-term care Medicaid?
1) What Is Medicaid Long-Term Care and How Does It Work? Medicaid, a needs-based healthcare program for people of all ages, pays for long-term care for elderly and handicapped people who fulfill their state’s qualifying criteria. This sort of service is available via a number of Medicaid programs. 28.02.2022
Does Medicaid pay for assisted living in Illinois?
For many Illinois residents, the Medicaid program pays for nursing homes, assisted living, and home health care. Nursing homes, assisted living facilities, and home health care are all pricey long-term care services in Illinois.
What is the new HSA limit for 2021?
HSA contributions will be capped at $3,600 for self-only coverage and $7,200 for family coverage. This is a 1.5 percent gain over the previous year.
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically enroll you in Medicare Parts A and B at the age of 65 if you are eligible. (The government Centers for Medicare & Medicaid Services runs Medicare, while Social Security manages enrollment.)
What happens if you contribute to an HSA while on Medicare?
You can no longer make contributions to an HSA after you enroll in Medicare. You may, however, utilize money from an HSA to cover certain Medicare expenditures. Once you enroll in Medicare, any money you put into an HSA will be subject to a tax penalty.
When should I stop contributing to my HSA?
A health savings account (HSA) is a kind of account that may be used to pay for medical expenses. If you have a high-deductible health plan, an HSA is usually included in your benefits. When should you cease making HSA contributions if you want to enroll in Medicare? The quick answer is that you should wait six months before applying for Medicare.
What age do you have to stop contributing to an HSA?
Most Americans lose their HSA eligibility when they turn 65 because they enter Medicare. The contribution for the last year is pro-rata.
Do I automatically get Medicare when I turn 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically enroll you in Medicare Parts A and B at the age of 65 if you are eligible. (The government Centers for Medicare & Medicaid Services runs Medicare, while Social Security manages enrollment.)
Conclusion
Watch This Video:
The “how do i get medicaid to pay for past medical bills” is a question that many people ask. The answer to the question is that you need to apply for Medicaid and have your nursing home doctor write an application letter.
Related Tags
- medicaid nursing home reimbursement rates by state 2021
- medicaid nursing home reimbursement rates by state 2020
- how to get medicaid to pay for a private room at nursing home
- how to submit unpaid medical bills to medicaid pa
- retroactive coverage medicaid