The Federal Medicaid Assistance Program
Contents
- Introduction to the Federal Medicaid Assistance Program
- How the Federal Medicaid Assistance Program Works
- Benefits of the Federal Medicaid Assistance Program
- Who is Eligible for the Federal Medicaid Assistance Program?
- How to Apply for the Federal Medicaid Assistance Program
- What Documents are Required to Apply for the Federal Medicaid Assistance Program?
- How to Renew Your Federal Medicaid Assistance Program Coverage
- What Changes can I make to my Federal Medicaid Assistance Program Coverage?
- What are the Costs of the Federal Medicaid Assistance Program?
- What are the Limitations of the Federal Medicaid Assistance Program?
The Federal Medicaid Assistance program provides financial assistance to eligible low-income adults, children, pregnant women, and people with disabilities who cannot afford health care
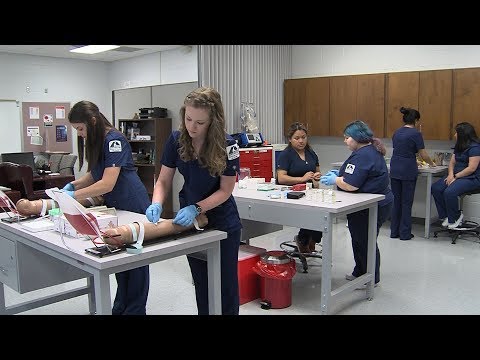
Checkout this video:
Introduction to the Federal Medicaid Assistance Program
The Federal Medicaid Assistance Program is a government assistance program that helps low-income individuals and families pay for medical care. The program is jointly administered by the federal government and each state’s government. Medicaid is the largest source of public funding for medical and health-related services in the United States
In order to be eligible for Medicaid assistance, an individual or family must meet certain income and resource requirements. income requirements vary from state to state, but generally speaking, an individual or family must have an income that does not exceed a certain percentage of the federal poverty level in order to qualify. In addition to income requirements, some states also have asset limits in place, which means that an individual or family’s savings and other assets must not exceed a certain value in order for them to qualify for Medicaid assistance.
Once an individual or family has been determined to be eligible for Medicaid assistance, they will be enrolled in a Medicaid managed care plan. Medicaid managed care plans are health insurance plans that contract with the state’s Medicaid program in order to provide coverage to enrollees. Enrollees are typically required to receive their Health Care services from providers who participate in the plan’s network, although some plans may offer out-of-network coverage as well.
How the Federal Medicaid Assistance Program Works
The federal Medicaid assistance program is a needs-based program that provides health care coverage to low-income individuals and families. Medicaid is jointly funded by the federal government and the states, and each state administers its own Medicaid program.
To be eligible for Medicaid, an individual must be a U.S. citizen or a legal immigrant, and must meet certain income and resource requirements. In general, Medicaid provides health care coverage for:
-Children under the age of 19
-Pregnant women
-Parents and caretakers of minor children
– Elderly adults (age 65+)
-Adults with disabilities
Benefits of the Federal Medicaid Assistance Program
The Medicaid program is a health insurance program for low-income individuals and families. The program is jointly funded by the federal government and the states, and it is administered by the states. Medicaid provides health coverage to millions of Americans, including children, pregnant women, parents, seniors, and people with disabilities.
Medicaid is an important source of health coverage for many low-income Americans. The program pays for a wide range of medical services, including doctor visits, prescription drugs, hospitalizations, laboratory tests, and preventive care. Medicaid also covers long-term care services such as nursing home care and personal care services for people with disabilities.
The Medicaid program is an important safety net for low-income Americans. Medicaid provides health coverage to millions of Americans who would otherwise be uninsured. In addition to providing health coverage, Medicaid also helps to reduce the financial burden of medical expenses for low-income families.
Who is Eligible for the Federal Medicaid Assistance Program?
The Federal Medicaid Assistance program is a need-based program that provides financial assistance to eligible low-income individuals and families to help cover the costs of medical and long-term care.
In order to be eligible for the Federal Medicaid Assistance program, an individual must meet certain income and asset requirements. Eligibility for the program is determined by each state, so requirements may vary from state to state. However, all states must adhere to the federal guidelines set forth by the Centers for Medicare and Medicaid Services (CMS).
To be eligible for Medicaid in most states, an individual’s income must not exceed 133% of the federal poverty level (FPL). For a family of four, this would be an annual income of about $32,000. In addition to meeting the income requirements, an individual must also have assets that fall below a certain limit. This asset limit varies from state to state, but is generally between $2,000 and $3,000 for an individual, or $4,000 and $6,000 for a family.
Certain groups of individuals are exempt from the asset limit test, including those who are disabled or blind, pregnant women, children under the age of 19, and adults over the age of 65. In addition, some states have expanded their Medicaid programs to cover additional groups of low-income individuals who do not typically qualify for need-based assistance programs like Medicaid. These groups may include childless adults, parents with dependent children, pregnant women with incomes above 133% FPL, and low-income adults ages 19-64.
How to Apply for the Federal Medicaid Assistance Program
In order to qualify for the Federal Medicaid Assistance Program, also known as FMAP, you must first meet certain criteria. To find out if you are eligible, contact your state Medicaid office. You can also visit the Medicaid website to get more information on program requirements.
If you qualify for FMAP, you will need to fill out an application and submit it to your state Medicaid office. Once your application has been reviewed and approved, you will be enrolled in the program and will begin receiving benefits.
What Documents are Required to Apply for the Federal Medicaid Assistance Program?
A complete and up-to-date list of the documents that are required for the application process for the federal Medicaid assistance program can be found on the official website for the program. However, some of the most commonly required documents include proof of income, tax returns, and identification documents.
How to Renew Your Federal Medicaid Assistance Program Coverage
You must renew your Medicaid coverage every year. The renewal process is different in each state, but usually involves filling out a form and providing proof of your continued eligibility.
To renew your Medicaid coverage, you will need to:
* Gather proof of your continued eligibility, which may include documents such as income tax returns, pay stubs, or Social Security disability award letters.
* Complete a renewal form, which is available from your state Medicaid office or online.
* Submit the completed renewal form and proof of continued eligibility to your state Medicaid office.
If you have any questions about renewing your Medicaid coverage, please contact your state Medicaid office
What Changes can I make to my Federal Medicaid Assistance Program Coverage?
Medicaid is a joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also covers children up to age 19 and pregnant women with incomes below 138% of the federal poverty level.
The Centers for Medicare & Medicaid Services (CMS) is the Federal agency that administers Medicaid. Each State has its own Medicaid program.
Coverage through the Federal Medicaid Assistance Program is different in each State. You should contact your State Medicaid office to find out what coverage is available in your State.
What are the Costs of the Federal Medicaid Assistance Program?
In order to be eligible for the Federal Medicaid Assistance program, states must agree to cover certain mandatory benefits, which vary slightly from state to state, as well as any optional benefits that the state chooses to cover. States are also required to cover certain groups of people who are deemed “medically needy” or “medically frail.”
The federal government provides assistance to states in two ways: through a block grant and through a matching program. The block grant is a fixed amount of money that the federal government provides to each state every year. The matching program is a cost-sharing arrangement in which the federal government reimburses states for a portion of the costs of providing Medicaid benefits.
In fiscal year 2015, the federal government’s share of Medicaid spending was $253 billion, or 62 percent of total Medicaid spending. The remainder was paid by state and local governments.
What are the Limitations of the Federal Medicaid Assistance Program?
There are a number of limitations to the Federal Medicaid assistance program. One of the primary limitations is that the program is only available to those who meet certain income requirements. In general, individuals and families who are at or below 138% of the Federal Poverty Level (FPL) will qualify for Medicaid assistance. However, there are some states that have expanded their Medicaid programs to include individuals and families above this income level.
Another limitation of the Federal Medicaid assistance program is that it is only available to citizens and legal residents of the United States. This means that undocumented immigrants are not eligible for Medicaid assistance, even if they meet all other eligibility requirements.
Finally, another limitation of the Federal Medicaid assistance program is that it does not cover all medical expenses. There are a number of services and treatments that are not covered by Medicaid, including dental care, vision care, and prescription drugs. Individuals who need coverage for these types of expenses may need to seek out other sources of financial assistance.