Continuity of Care is a Pillar of Acos and Patient Centered Medical Home Models.
Contents [show]
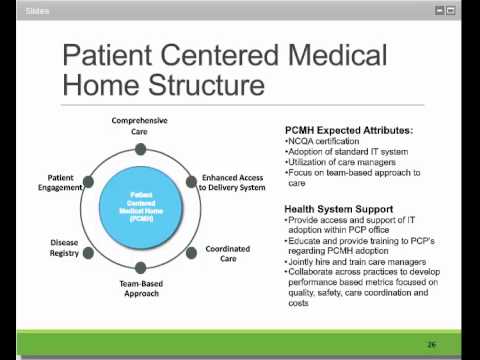
The Patient Centered Medical Home model is a well-established and widely used health care delivery system that focuses on the patient as the key decision maker. It’s a model that has been proven effective in improving outcomes, reducing costs, and increasing satisfaction for patients. However, it relies heavily on continuity of care to maintain its effectiveness. This article discusses how continuous care can be achieved through medical home models.
The Continuity of Care is a Pillar of Acos and Patient Centered medical home Models. near Iowa is a pillar that must be present in order to have an effective medical home. It’s not just the doctor, it’s also the nurse, social worker, and other staff members who all work together to ensure the patient has access to care.
This Video Should Help:
What is continuity of care?
Continuity of care is a central tenet of both the patient centered medical home (PCMH) and the accountable care organization (ACO) models of care. Simply put, it is the idea that patients should have ongoing relationships with a small team of caregivers who can provide them with comprehensive, coordinated care over time.
There is a growing body of evidence that continuity of care leads to improved health outcomes and lower costs, making it a key quality metric for both ACOs and PCMHs. In one recent study, continuity of care was found to be associated with better management of chronic diseases, lower rates of hospitalization and emergency department use, and more appropriate use of medications. Continuity of care has also been linked to higher patient satisfaction scores and better engagement in their own health.
Despite these well-documented benefits, continuity of care remains elusive for many patients due in part to our fragmented healthcare system. To further complicate matters, there is currently no standard definition of continuity of care, making it difficult to measure and compare across different health plans and provider organizations.
If we are to realize the full potential of ACOs and PCMHs, it is essential that we invest in research to better understand continuity of care and how we can make it a reality for more patients. In the meantime, payers and provider organizations should continue to work together to find ways to promote continuity of care within their own networks.
Why is continuity of care important?
There is a growing body of evidence that continuity of care is associated with better health outcomes, including improved quality of care, fewer hospitalizations and Emergency Department visits, and lower mortality rates. In addition, continuity of care has been linked to higher patient satisfaction scores. Given the importance of continuity of care to patient health and satisfaction, it is not surprising that it is a key element of both the accountable care organization (ACO) and patient-centered medical home (PCMH) models of care.
There are a number of reasons why continuity of care is so important. First, it helps to ensure that patients receive the necessary follow-up care after a hospitalization or other episode of care. This is especially important for patients with chronic conditions, who may require ongoing management in order to prevent complications. Second, continuity of care helps to build trust between patients and their caregivers. When patients see the same doctor or nurse over time, they are more likely to feel comfortable discussing sensitive issues and to feel confident that their needs will be met. Finally, continuity of care can help to improve coordination among different caregivers, leading to better overall coordination of care.
While the importance of continuity of care is clear, there are some challenges associated with providing it. First, it can be difficult to maintain continuity when patients move between different providers or settings (e.g., from the hospital to a nursing home). Second, providing continuity often requires additional time and resources from providers, which may not be reimbursed under traditional fee-for-service models. As a result, many providers are reluctant to invest in providing continuity of care unless they are confident that they will be compensated for doing so.
Despite these challenges, there is a growing recognition that continuity of care is essential to providing high-quality patient-centered care. As a result, ACOs and PCMHs are increasingly likely to include Continuity of Care as one of their key pillars.
What are the benefits of continuity of care?
Patient-centered medical care is a model of care in which patients play a central role in their own health care. This approach to care focuses on continuity of care, comprehensive care, and coordination of care.
Continuity of care is a key component of both the Patient Centered Medical Home (PCMH) and Accountable Care Organization (ACO) models of health care delivery. In these models, patients have a ufffdmedical homeufffd ufffd a primary care provider or team of providers ufffd who coordinate all aspects of the patientufffds care. The goal is to provide high-quality, coordinated, patient-centered care that is more efficient and effective than traditional fee-for-service medicine.
There is strong evidence that continuity of care leads to improved health outcomes for patients. A 2012 systematic review of the impact of continuity of care on quality and cost found that continuity of care was associated with better self-reported health, lower rates of hospitalization and emergency department visits, and lower costs. However, the authors cautioned that more research is needed to determine the optimal way to deliver continuity of care.
One challenge in delivering continuity of care is funding. Continuity of care requires an ongoing relationship between patients and their providers, which can be expensive to maintain. In addition, many insurers reimburse based on fee-for-service, which rewards episodic or one-time interactions rather than ongoing relationships. As a result, it can be difficult for providers to generate enough revenue to cover the costs associated with continuity of care.
Despite these challenges, continuity of care is considered an important component of high-quality health care. If you are interested in learning more about this topic, please see the attached article from The Hastings Center Report titled ufffdContinuity of Care: A Pillar of ACOs and Patient-Centered Medical Homesufffd by James Salwitz, MD. This article provides an overview of the benefits of continuity of care and discusses some strategies for funding this type of care.
How can continuity of care be improved?
Medicare’s Patient-Centered Medical Home (PCMH) and Accountable Care Organization (ACO) models are based on the delivery of coordinated, continuous, patient-centered care. A key goal of these models is to improve patient care quality and outcomes while controlling costs.
Continuity of care is a key driver of improved patient outcomes and lower costs. A systematic review of the literature on continuity of care found that patients who received continuity of care had better health outcomes, including fewer hospitalizations and emergency department visits, than those who did not receive continuity of care.1 In addition, a number of studies have found that continuity of care is associated with lower costs.2-4
There are a number of ways to improve continuity of care, such as providing patients with access to their medical records, coordinating care among different providers, and improving communication between providers and patients.5-7 However, one of the most effective ways to improve continuity of care is through provider communication and collaboration.8-10
Provider communication and collaboration can be improved through the use of health information technology (HIT), such as electronic health records (EHRs). EHRs can help providers share information with each other and with patients, which can improve coordination of care.11-13 In addition, EHRs can help providers track patientsufffd progress over time, which can improve continuity of care.14
Despite the potential benefits of HIT for continuity of care, there are challenges that need to be addressed in order for HIT to be used effectively for this purpose.15 One challenge is that provider organizations need to have the infrastructure in place to support HIT use, such as robust broadband connectivity and adequate staffing levels.16 In addition, provider organizations need to ensure that their EHR systems are interoperableufffdthat is, they can exchange data with other systemsufffdin order to facilitate information sharing.17 Another challenge is that provider organizations need to have the capacity to effectively use HIT tools in order to improve continuity of care.18 This includes having staff who are trained in how to use HIT tools and having policies and procedures in place that support HIT use.19
Despite these challenges, provider organizations that are able to effectively use HIT will be well positioned to improve continuity of care and deliver high-quality, coordinated patient-centered care.
What are the challenges to continuity of care?
Research shows that continuity of care is a key predictor of improved patient outcomes and satisfaction, yet it can be difficult to achieve in real-world settings. One challenge is that continuity of care requires close coordination between different types of providers, which can be hard to achieve in a traditional fee-for-service environment. Another challenge is that continuity of care can be time-consuming and costly, so it may not be feasible for all patients.
In recent years, there has been a move towards value-based models of care delivery, such as the Patient Centered Medical Home (PCMH) model. These models seek to improve the quality of care while reducing costs, and one of the key pillars of these models is continuity of care. However, there are still challenges to implementing these models effectively, such as lack of funding and provider buy-in.
What are some solutions to challenges to continuity of care?
When it comes to providing high-quality patient care, continuity of care is a key pillar. Unfortunately, there are many challenges that can impede continuity of care, including changes in insurance coverage, provider turnover, and patients’ own preferences and schedules.
One potential solution to these challenges is the Patient Centered Medical Home (PCMH) model. This model of care puts the patient at the center of their care team, which can help to ensure that each patient receives the coordinated and continuous care they need. Another solution is Acos (Accountable Care Organizations), which are groups of providers that accept financial responsibility for the quality and cost of care for a defined population of patients.
Of course, funding is always a major challenge when it comes to providing high-quality patient care. Research continues to be an important part of finding new and innovative solutions that can improve continuity of care while also reducing costs. Citation: Continuity of Care Is a Pillar of ACOs and Patient-Centered Medical Home Models – Health Affairs
How can providers ensure continuity of care?
Providers can ensure continuity of care by making sure they have adequate staffing, by training staff to deliver care that is consistent with the medical home model, and by investing in care coordination and case management resources. In addition, provider organizations can seek out funding opportunities to support the implementation of the medical home model and can participate in research to help identify best practices for delivering continuity of care.
What role do patients play in continuity of care?
One of the key components of the Patient Centered Medical Home (PCMH) model of care is continuity of care. Continuity of care is defined as “the degree to which patients receive consistent care from a medical team over time” and has been shown to be associated with improved quality and patient satisfaction. However, the role that patients play in continuity of care has not been well studied.
A recent study published in the Journal of General Internal Medicine sought to fill this gap in our knowledge by examining how patients’ involvement in their own care affects continuity of care. The study found that patients who were more engaged in their own care (e.g., those who made appointments for themselves, kept track of their own health information, etc.) were more likely to have continuity of care with their primary care provider.
This study provides important insights into how we can improve continuity of care for our patients. It also highlights the importance of patient engagement in their own care, which is another key component of the PCMH model.
What are the implications of continuity of care?
The implications of continuity of care are far-reaching, and its importance is increasingly recognized in the health care industry. In short, continuity of care is the constant provision of medical care from a single provider or group of providers. This means that patients have uninterrupted access to care from the same providers throughout their course of treatment.
There are many benefits to continuity of care, both for patients and for providers. For patients, continuity of care has been shown to improve health outcomes, increase patient satisfaction, and reduce health care costs. For providers, continuity of care can lead to increased job satisfaction and decreased turnover rates.
Despite the many benefits of continuity of care, there are still some challenges that need to be addressed. One challenge is funding. Many Acos and Patient Centered Medical Home (PCMH) models are based on providing continuous care to patients, but these models often lack the necessary funding to sustain them. Another challenge is citation. Continuity of care is often under-cited in medical research, making it difficult for providers to find information about its benefits.
Despite these challenges, continuity of care is a vital part of many health care delivery models, and its importance will continue to grow in the coming years.
What are the future directions for continuity of care?
There is a large body of evidence demonstrating that continuity of care is associated with improved clinical outcomes, including lower mortality rates, fewer hospitalizations, and better management of chronic diseases. In addition, patients who have a continuous relationship with a primary care provider are more likely to receive preventive care services and to be more satisfied with their care.
The Patient-Centered Medical Home (PCMH) model of care delivery is based on the principle of continuity of care, and many Accountable Care Organizations (ACOs) are also incorporating continuity of care into their models. Given the growing interest in these models of care delivery, it is important to understand the future directions for research on continuity of care.
One important direction for future research is to examine the impact of continuity of care on quality of life and patient satisfaction. In addition, there is a need for more studies that examine the cost-effectiveness of continuity of care, as this is an important consideration for ACOs and other health care organizations. Another key area for future research is to identify ways to improve continuity of care for vulnerable populations, such as those with chronic mental illness or multiple chronic conditions.
Finally, it is important to continue to monitor the effects of policy changes on continuity of care. For example, Medicare funding cuts have led to reductions in ContinuityofCare.org’s annual survey sample size and numberof participating practices. As policy changes occur, it will be crucialto assess their impact on continuity of care so that we can identify effective strategies for preserving this important elementof high-quality health care.
The “patient-centered medical home examples” is a pillar of the Acos and Patient Centered Medical Home Models. The goal of these models is to provide continuity of care for patients and their families, which helps reduce costs, improve health outcomes, and increase quality of life.